Thousands of dollars in Federal Grant Assistance are available to help you recover. Whether it’s emergency rental aid or utility relief, 2026 programs are designed to provide a safety net for your family. See what you qualify for in minutes.
Apply for AssistanceDoes medicaid cover braces is a common question, and the answer is often yes, particularly for children, but it comes with important conditions. The primary determining factor for coverage is "medical necessity". This means that Medicaid, as a health insurance program, typically covers treatments deemed essential for an individual's health, rather than for purely cosmetic improvements.
Coverage for braces through Medicaid is most frequently available for individuals under the age of 21. This is largely due to federal mandates associated with child health programs, which aim to provide comprehensive care during developmental years. For adults seeking orthodontic treatment, Medicaid coverage is significantly more restricted and varies considerably from state to state, with many states not offering this benefit to the adult population at all. Understanding these fundamental distinctions is the first step in determining potential eligibility for Medicaid-funded orthodontic care.
The term "medically necessary" is the cornerstone of Medicaid's decision-making process for orthodontic coverage. For braces to be considered medically necessary, they must be required to correct or improve a significant dental health problem that adversely affects an individual's overall health, ability to function, or proper development. It's not enough for teeth to be simply misaligned; the condition must lead to identifiable health issues or functional impairments.
Several types of conditions are often evaluated for medical necessity. These frequently include:
It is important to recognize that orthodontic treatment solely for cosmetic reasons, such as correcting mildly crooked teeth that do not pose health or functional problems, is generally not covered by Medicaid. To ensure objectivity in these assessments, many states employ specific guidelines or scoring systems. One common tool is the Handicapping Labio-Lingual Deviation (HLD) Index, while other states may use a list of automatically qualifying conditions to determine if the severity of the malocclusion warrants coverage.
This structured approach means the decision isn't arbitrary but based on defined criteria that the orthodontist must document thoroughly, aligning the patient's condition with state-specific requirements. The focus remains firmly on addressing functional impairments like difficulty chewing or speaking, or preventing more serious dental diseases, rather than purely aesthetic improvements.
Table 1: Common Conditions That May Qualify Braces as Medically Necessary Under Medicaid
| Condition Category | Examples/Specifics | General Medicaid Consideration |
|---|---|---|
| Severe Malocclusion | Deep impinging overbite, severe underbite (reverse overjet >3.5mm), posterior crossbite of multiple teeth, overjet >9mm | Must cause functional issues (chewing, speech) or risk tissue damage. Assessed by severity. |
| Craniofacial Anomalies | Cleft palate, hemifacial microsomia | Often automatically qualifying or given high priority due to significant impact on development and function. |
| Functional Impairment | Difficulty eating, swallowing, or speaking due to jaw misalignment or dental issues | The impairment must be directly linked to the orthodontic condition and correctable with braces. |
| Impacted Permanent Teeth | Anterior teeth (incisors, cuspids) unable to erupt, extraction not viable | Condition must impede normal dental development; orthodontic intervention planned to bring teeth into arch. |
| Severe Crowding/Spacing | Extreme lack of space or excessive gaps leading to inability to maintain oral hygiene, severe decay, or gum disease | Must demonstrate a direct link to oral health problems that cannot be managed by other means. |
| Traumatic Dental Injuries | Loss or displacement of teeth/jaw segments due to accidents or burns | Orthodontic treatment as part of necessary reconstruction to restore function and dental integrity. |
Children and adolescents under the age of 21 who are enrolled in Medicaid generally have a more extensive entitlement to dental services, which includes medically necessary orthodontics. This broader coverage is primarily delivered through the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit. The EPSDT program is a comprehensive and preventive child health initiative designed to ensure that children receive appropriate health care, including dental care, early in life.
A key aspect of EPSDT is its mandate that states must provide any service necessary to "correct or ameliorate" a physical or mental defect or condition discovered during a screening, even if that specific service (like certain orthodontic procedures) is not covered for the adult Medicaid population in that particular state. This provision can be particularly powerful for accessing orthodontic care. However, even under the robust EPSDT benefit, the principle of "medical necessity" remains paramount.
The orthodontic condition must be significant enough to warrant treatment based on the state's established criteria. The term "ameliorate" suggests an improvement or making a condition more bearable, which could theoretically extend to the psychosocial impacts of severe dental issues, though coverage decisions often lean more heavily on demonstrable physical or functional impairments.
Regular dental check-ups are an integral part of the EPSDT benefit. These routine visits are crucial because they can be the point at which orthodontic problems are first identified by a dentist, leading to a referral to an orthodontist for further evaluation. Early identification and intervention, a core tenet of EPSDT, can sometimes lead to more effective and less complex orthodontic treatment, potentially preventing more severe issues from developing later on.
The age limit for EPSDT benefits, and thus for this enhanced access to medically necessary orthodontics, is typically up to age 21, although minor variations might exist in how states manage program termination at this age. While EPSDT offers a strong federal pathway, its practical application for orthodontics is still shaped by state-level definitions and interpretations of medical necessity.
When it comes to Medicaid coverage for braces for adults, typically defined as individuals age 21 and over, the landscape is markedly different and far more restrictive. It is crucial to understand that while states are federally mandated to provide a comprehensive set of dental benefits to children through the EPSDT program, adult dental services, including orthodontics, are considered optional for states to offer under Medicaid. This fundamental policy difference is the primary reason why adult orthodontic coverage through Medicaid is rare.
According to a 2021 analysis, only a very small number of states—specifically three—provided orthodontic coverage for their general adult Medicaid population. While state policies can change over time, this figure highlights the general scarcity of such benefits for adults. Individuals seeking this information should have very low expectations and must verify the current policies of their specific state's Medicaid program. Even in states that might technically offer adult orthodontic benefits, the eligibility criteria are likely to be exceptionally stringent.
If an adult presents with an extremely severe condition, such as a craniofacial anomaly resulting from a significant accident or a condition that profoundly impairs essential life functions like eating or speaking, there might be a slim possibility of coverage in some states. Such cases would almost certainly be evaluated on a case-by-case basis and would require extensive documentation and review, with the bar for "medical necessity" set extraordinarily high. Orthodontic treatment pursued for primarily cosmetic reasons by adults is virtually never covered by Medicaid.
Some states may offer expanded dental benefits, potentially including orthodontics in rare, highly medically necessary circumstances, for specific adult groups such as pregnant women or adults with certain disabilities, but this is not a widespread practice and should not be assumed. The optional nature of adult dental benefits means that orthodontics, often viewed as costly, is frequently excluded or severely limited in state Medicaid plans for adults.
Navigating the process to obtain Medicaid coverage for braces involves several key steps, requiring diligence from both the patient or guardian and the dental provider. The journey typically begins long before an orthodontic consultation.
While the orthodontist's office typically manages the submission of the PA request, it is beneficial for the patient or their guardian to be aware of this critical process and to cooperate fully in providing any needed information. The prior authorization step serves as the primary mechanism for Medicaid to control costs and ensure that covered orthodontic services strictly adhere to the established criteria for medical necessity.
Table 2: General Steps for Medicaid Prior Authorization for Braces
| Step | Description | Key Considerations/Documentation |
|---|---|---|
| 1. Orthodontic Evaluation | A Medicaid-enrolled orthodontist assesses the patient's dental condition. | Determines if the condition is severe enough to potentially meet Medicaid's medical necessity criteria. |
| 2. Medical Necessity Determination | Orthodontist applies state-specific criteria (e.g., HLD Index, auto-qualifying conditions) to the patient's case. | Objective measurements, scores, and specific diagnoses are recorded. |
| 3. Compilation of PA Packet | Orthodontist's office gathers all required documentation for the prior authorization request. | Includes patient demographics, Medicaid ID, treatment plan, diagnostic records (X-rays, models/scans, photos), and a narrative justifying medical necessity. |
| 4. Submission of PA Request | The orthodontist submits the complete PA packet to the state Medicaid agency or its dental benefits administrator. | Submission is often electronic via a provider portal, but fax may be an option. Accuracy and completeness are crucial. |
| 5. Medicaid Review | Medicaid reviewers (often dental consultants) evaluate the PA request against state guidelines and medical necessity standards. | May involve checking HLD scores, verifying qualifying conditions, and ensuring all documentation is adequate. Incomplete requests may be returned or denied. |
| 6. Decision (Approval or Denial) | Medicaid issues a formal decision. | Approvals come with an authorization number valid for a specific period. Denials include reasons and information on appeal rights. |
| 7. Communication of Decision | The orthodontist and/or patient/guardian are notified of the decision. | If approved, treatment can be scheduled. If denied, options for appeal can be considered. |
When Medicaid approves orthodontic treatment based on medical necessity, the coverage typically extends to standard procedures and services required to correct the qualifying dental health condition. The primary goal is to restore function and oral health in a cost-effective manner. Generally, this includes:
It is important to understand that services considered primarily cosmetic or those that offer aesthetic advantages without a significant medical benefit over standard treatment are generally not covered by Medicaid. This often means:
The specifics of covered orthodontic services, including any limitations or exclusions, can vary from one state to another. Therefore, it is always advisable for the patient or their guardian to confirm the details of what is and is not covered with both the Medicaid-enrolled orthodontist and, if necessary, directly with their state's Medicaid plan before commencing treatment. This ensures clarity and helps avoid unexpected out-of-pocket expenses.
Receiving a denial for Medicaid coverage for braces can be disheartening, but it is important to know that individuals generally have the right to appeal this decision. The appeals process provides an opportunity to have the case reviewed again, potentially by a different set of reviewers or a hearing officer.
The general steps involved in appealing a Medicaid denial for orthodontic treatment are as follows:
It's worth noting the concept of "aid paid pending," which allows Medicaid benefits to continue during an appeal. However, this typically applies when existing benefits are being reduced or terminated. For a denied request for a new service like braces, aid paid pending is usually not applicable, meaning Medicaid will not pay for the braces while the appeal for initial coverage is underway. The appeals process, while a right, requires careful attention to detail, timely action, and a clear presentation of why the orthodontic treatment is medically necessary according to Medicaid's own standards.
It is a reality that not every individual seeking braces will qualify for Medicaid coverage, particularly adults or those whose conditions do not meet the stringent "medical necessity" criteria. When Medicaid is not an option, several alternative avenues can help manage the cost of orthodontic treatment:
Exploring these alternatives requires proactive research and financial planning. For many families, a combination of these strategies may be necessary to make orthodontic treatment achievable when Medicaid coverage is not available.
Navigating Medicaid and understanding orthodontic benefits can be complex, as program details vary significantly from state to state. For the most accurate and comprehensive information, it is recommended to consult official sources:
Because Medicaid is administered at the state level, the rules, eligibility criteria, and specific covered services (including the details of orthodontic benefits) can differ substantially. Therefore, the single most important resource is the official Medicaid website for an individual's specific state. These state-specific portals provide the most current and locally relevant information.
Additionally, individuals can contact their local county assistance office or the state's Medicaid helpline if they have questions about their eligibility, the application process, or the specifics of dental and orthodontic coverage in their area. These direct lines of communication can often provide personalized assistance.
Medicaid may cover braces if they are deemed medically necessary, meaning they are needed to correct a severe misalignment that affects oral health, speech, or chewing. Coverage specifics vary significantly by state.
Federal law requires Medicaid to cover medically necessary dental services for children under the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit. This often includes braces for significant orthodontic issues.
Generally, severe malocclusions such as significant overbites, underbites, crossbites, extreme crowding, or misalignment affecting function (chewing, speech) are considered medically necessary. Cosmetic issues are typically not covered.
Coverage for adult orthodontic treatment is much more limited and varies greatly by state. Some states may offer coverage for adults if braces are medically necessary for specific health reasons, such as preparation for surgery.
The best way is to contact your state's Medicaid agency directly. Their website or a phone representative can provide detailed information on covered services and eligibility requirements for orthodontic treatment.
If full coverage isn't available, explore payment plans with the orthodontist, other financing options, or community programs that may offer assistance with orthodontic costs. Some dental schools also offer lower-cost treatment.
Even if Medicaid covers traditional braces, it may not cover clear aligners, which are often considered a cosmetic alternative. Coverage for specific types of orthodontic appliances varies.
Schedule a consultation with an orthodontist who accepts Medicaid. They can evaluate your child's orthodontic needs and help determine if the treatment is considered medically necessary and if Medicaid might provide coverage.
Yes, coverage for children usually extends up to age 21 under the EPSDT benefit. Adult coverage, where it exists, may have different criteria and limitations.
The Children's Health Insurance Program (CHIP) also often covers dental services, including orthodontics, if deemed medically necessary. Check your specific CHIP plan details for coverage information.
The question of does applebees take ebt is common for those wanting to use Supplemental Nutrition Assistance Program (SNAP) benefits for a restaurant meal. The direct answer is that Applebee's restaurants do not accept Electronic Benefit Transfer (EBT) cards for meals. This policy applies to their locations nationwide.
Understanding SNAP and Restaurant Meals
While this might be disappointing, SNAP benefits are mainly for buying unprepared food. However, programs like the Restaurant Meals Program (RMP) allow certain eligible SNAP recipients to use EBT cards at authorized restaurants. Applebee's official website, in its payment methods and gift card sections, doesn't list EBT as accepted. This aligns with information from other sources stating their non-acceptance of EBT.
The main reason Applebee's and similar full-service restaurants usually don't accept EBT cards relates to SNAP's core purpose. SNAP helps low-income individuals and families buy eligible food for home preparation from places like grocery stores. Hot, prepared foods, like those at Applebee's, are generally not covered by standard SNAP EBT rules.
Factors Influencing Applebee's Decision
Several factors likely contribute to Applebee's choice not to accept EBT, even where the Restaurant Meals Program (RMP) exists:
What is the RMP?
The Restaurant Meals Program (RMP) is a key aspect to understand when discussing EBT at restaurants. It's a state-run SNAP option, overseen by the U.S. Department of Agriculture's Food and Nutrition Service (FNS). It lets certain SNAP recipients buy prepared meals at approved restaurants with their EBT cards. The RMP aims to help vulnerable SNAP clients who can't prepare their own meals or lack stable housing for food storage and preparation, providing access to hot, nutritious meals.
Who Qualifies for RMP?
Not all SNAP recipients are eligible for the RMP. It specifically targets these groups :
State SNAP agencies identify eligible households. Their EBT cards are specially coded for use at RMP-participating restaurants. If a SNAP recipient isn't in one of these categories, they can't use their EBT card for restaurant meals, even in an RMP state at a participating restaurant.
How Restaurants Join the RMP
For a restaurant to accept EBT through the RMP, it must meet several conditions :
Each state can also set its own rules for choosing participating restaurants. This state-level control means RMP availability and operations vary, which can be complex for national chains.
RMP Availability
The Restaurant Meals Program isn't available everywhere; states decide whether to offer it. As of early 2025, these states have an active RMP, though the coverage (statewide or specific counties) can differ :
Applebee's Participation Status
Despite these states having RMPs, checks of official state RMP participant lists and related resources show Applebee's is NOT currently listed as a participating restaurant in any of them. For people in these states, it's vital to check official state resources for the latest list of approved RMP vendors.
State RMP Details and Contacts
The table below summarizes RMP participation by state and gives links to official state program information or contacts. This helps users verify details and check for updates, as RMP participation can change.
| State | Participates in RMP? | Applebee's Listed in State RMP? | Official State RMP Information Link/Contact |
|---|---|---|---|
| Arizona | Yes (Statewide) | No | Email: FAAMOU@azdes.gov or Phone: 602-774-9284 |
| California | Yes (Statewide) | No (based on general checks) | (https://www.cdss.ca.gov/rmp) or Email:(mailto:CDSSRMP@dss.ca.gov) |
| Illinois | Yes (Cook & Franklin Counties) | No | Email:(mailto:DHS.RMP@illinois.gov) or Phone: 217-558-7757 |
| Maryland | Yes | No | (https://dhs.maryland.gov/restaurant-meals-program/) or Email: shanise.smith@maryland.gov |
| Massachusetts | Yes (Statewide) | No | (https://www.mass.gov/info-details/list-of-restaurantsfood-trucks-approved-by-the-commonwealth-of-massachusetts-for-the-snap-restaurant-meals-program-rmp) or Email:(mailto:DTA.RMP@mass.gov) |
| Michigan | Yes | No | (https://www.michigan.gov/mdhhs/assistance-programs/food/restaurant-meal-program) or Email: mdhhs-restaurantmealprogram@michigan.gov |
| New York | Yes (Expanding, some counties) | No (based on general checks) | (https://otda.ny.gov/programs/rmp/) or Email: susan.zimet@otda.ny.gov |
| Rhode Island | Yes | No | (https://dhs.ri.gov/programs-and-services/supplemental-nutrition-assistance-program-snap/supplemental-nutrition-5) or Email: jenna.simeone@dhs.ri.gov |
| Virginia | Yes | No | (https://www.dss.virginia.gov/vrmp/locations.cgi) or Email: vrmp@dss.virginia.gov |
For the most thorough information on state RMP programs, the USDA Food and Nutrition Service website is a key resource.
Checking Official Resources
For SNAP recipients meeting RMP criteria (elderly, disabled, or homeless), finding participating local restaurants means checking official state or county resources. There isn't one national database of all RMP restaurants because states, and sometimes counties, manage the program.
Methods for Locating RMP Restaurants
Here’s how to find RMP-approved restaurants:
Information on RMP restaurants is scattered, so relying on official state and local government sources is best.
Exploring Other Options
Since Applebee's isn't in the RMP, eligible SNAP recipients needing restaurant options must look elsewhere. The types of RMP-participating restaurants vary but often include:
Important Verification Note
It's crucial to remember that a chain's name here doesn't guarantee any specific location accepts EBT. Participation depends on the state, county, and individual restaurant's authorization. Always check official state RMP lists or contact the restaurant directly before trying to use EBT. The RMP provides a prepared meal experience, different from using EBT at grocery stores for items to cook at home.
Primary Use of EBT Cards
Beyond restaurant meals, EBT cards are the main way SNAP recipients access food benefits for many eligible purchases. Most commonly, EBT is used for unprepared food at authorized retailers, such as:
Online EBT Purchases
Also, more online grocery retailers and delivery services are now authorized to accept EBT for online purchases of eligible food. Major retailers like Amazon, Walmart, and Aldi allow online EBT purchasing in many states. Note that SNAP benefits usually cover only eligible food costs, not delivery fees, service charges, or other non-food items with online orders.
Here's a summary of key information about Applebee's and EBT cards:
For those eligible for the RMP, checking these official state resources is the best way to find dining options where EBT benefits can be used for prepared meals.
Generally, no. Applebee's restaurants typically do not accept EBT cards as a form of payment for dine-in or standard takeout orders.
BT cards are primarily intended for purchasing groceries and essential food items at authorized retailers. Restaurants like Applebee's usually don't qualify under these guidelines.
In very specific situations, such as if an Applebee's is located within a grocery store or participates in a state-run Restaurant Meals Program (RMP) for eligible individuals like the elderly or disabled, EBT might be accepted. However, this is rare.
The RMP is a state option within the SNAP (Supplemental Nutrition Assistance Program) that allows certain individuals who might have difficulty preparing meals themselves to use their EBT benefits at participating restaurants. Not all states have this program, and not all restaurants participate.
The best way to check is to directly contact the specific Applebee's location you plan to visit and inquire about their payment options, specifically mentioning the Restaurant Meals Program if you believe you might be eligible.
Applebee's usually accepts major credit cards (Visa, Mastercard, American Express, Discover), debit cards, Apple Pay, Google Pay, and cash. They may also accept Applebee's gift cards.
Restaurants that participate in the RMP are more likely to be fast-food establishments or smaller, local eateries rather than large chain restaurants like Applebee's.
You can check your state's SNAP agency website for a list of participating RMP restaurants, if your state has such a program. You might also find local community resources that provide this information.
While it's difficult to say definitively, it's not a common practice for full-service restaurants like Applebee's to accept EBT for regular purchases, as it goes against the program's primary purpose. Any future changes would likely depend on shifts in federal or state SNAP regulations and Applebee's business decisions.
If you are facing food insecurity, you can reach out to local food banks, soup kitchens, and social service agencies for support. These resources can provide meals and connect you with other assistance programs.
The question of "does popeyes take ebt" is common among those using food assistance. Typically, Popeyes, like most fast-food outlets, cannot accept Electronic Benefit Transfer (EBT) for hot, prepared foods under standard Supplemental Nutrition Assistance Program (SNAP) rules. However, a specific state-run program called the Restaurant Meals Program (RMP) creates a possibility for EBT use at select Popeyes locations for eligible individuals.
Whether a particular Popeyes accepts EBT depends on a few key conditions:
This means a straightforward "yes" or "no" isn't possible, as EBT acceptance at Popeyes varies by location and individual eligibility. While standard SNAP is for groceries, the RMP caters to those who cannot easily prepare their own food. Because RMP is a state option and restaurants opt-in, there isn't a universal Popeyes EBT policy.
To grasp how Popeyes might accept EBT, it's essential to know what EBT and SNAP are. EBT (Electronic Benefit Transfer) is the electronic system states use to deliver benefits like SNAP. An EBT card works like a debit card for accessing these benefits.
SNAP (Supplemental Nutrition Assistance Program) is a federal USDA program providing food aid to eligible low-income individuals and families. Its main purpose is to help households afford nutritious food for home preparation.
What SNAP Typically Covers
Generally, SNAP benefits can buy:
What SNAP Typically Excludes
SNAP benefits usually cannot purchase:
The exclusion of hot, prepared foods is why fast-food restaurants like Popeyes generally don't accept EBT under standard SNAP rules. This distinction highlights the need for programs like the RMP for those unable to cook at home.
The Restaurant Meals Program (RMP) is a vital exception to standard SNAP rules. It allows certain vulnerable SNAP recipients to buy prepared meals at authorized restaurants using their EBT cards.
What is the RMP?
The RMP is a state-level option within SNAP. It serves individuals who can't prepare their own meals or lack stable housing for food preparation. The USDA's Food and Nutrition Service (FNS) oversees SNAP federally, while states manage it locally, including deciding whether to implement an RMP.
Who Qualifies for the RMP?
RMP eligibility targets specific SNAP recipient groups. Generally, all household members must meet criteria, or it applies to an individual and their qualifying spouse. Key eligible groups include:
States may have specific processes for RMP certification. These criteria acknowledge that food insecurity affects different people in different ways.
Table 1: Who Qualifies for the Restaurant Meals Program (RMP)?
| Eligibility Group | General Criteria |
|---|---|
| Elderly | 60 years of age or older. |
| Disabled | Receives qualifying disability payments or benefits from a governmental agency due to a permanent disability. |
| Homeless | Lacks a fixed, regular, and adequate nighttime residence. |
| Eligible Spouse | Spouse of an RMP-eligible SNAP recipient, often under specific household composition rules. |
How RMP Works for SNAP Recipients
For eligible SNAP recipients, their EBT cards are usually specially coded by the state for RMP transactions. The restaurant doesn't determine eligibility; the EBT system handles it. This simplifies point-of-sale transactions.
In states like New York, recipients can check RMP status via online portals like ebtEDGE. If you believe you qualify but aren't coded, contact your local social services office. Typically, a separate RMP application isn't needed; state agencies should update cases.
Popeyes' stance on EBT is tied to its RMP participation.
Why Popeyes and EBT Isn't Simple
Popeyes primarily sells hot, prepared meals, so it generally doesn't accept EBT under standard SNAP. Any EBT acceptance at Popeyes is almost always through a state's RMP. Some sources say Popeyes doesn't take EBT (true for general SNAP), while others note limited RMP participation. Popeyes corporate doesn't have a universal RMP policy; it seems to be a state and franchisee decision.
States with the Restaurant Meals Program
RMP availability varies. As of early to mid-2025, participating states often include:
This list can change, and details (like county limits) vary. Always verify with your state's SNAP agency. The USDA FNS website offers RMP information and state contacts.
Popeyes' RMP Participation: What We Know
Evidence of Popeyes' RMP participation is localized and inconsistent:
Popeyes' RMP participation is limited and location-dependent, likely influenced by individual franchisee decisions.
Table 2: States with Restaurant Meals Programs and Notes on Popeyes
| State | RMP Active? | Popeyes RMP Participation Noted in Sources? |
|---|---|---|
| Arizona | Yes | Yes, general mention as a participating chain |
| California | Yes | Yes, general mention; anecdotal reports of varied local participation |
| Illinois | Yes, in limited counties/zip codes (Cook, Franklin) | Yes, potentially in designated RMP areas |
| Maryland | Yes | Yes, general mention as a participating chain |
| Massachusetts | Yes | Potentially, included in some broad national lists |
| Michigan | Yes | Yes, specific mention of Grand Rapids; general participation noted |
| New York | Yes | Yes, specific Brooklyn locations listed as participating |
| Rhode Island | Yes | Yes, general mention as a participating chain |
| Virginia | Yes | Yes, general mention as a participating chain |
How to Confirm if Your Local Popeyes Accepts EBT via RMP
To confirm EBT acceptance at a specific Popeyes through RMP:
Verification often falls on the SNAP recipient.
If a Popeyes participates in RMP and you're eligible, you can buy prepared meals. This typically includes items from Popeyes' regular menu like chicken, sandwiches, and sides. The RMP focuses on "prepared meals," unlike standard SNAP's grocery focus.
Remember, even under RMP, SNAP benefits cannot buy:
Some states' RMPs (like New York and Maryland) may offer meals at discounted prices, but this isn't universal. The EBT transaction covers eligible food costs.
Tips for Using EBT at RMP-Approved Restaurants
For a smoother RMP experience:
If your local Popeyes isn't in the RMP, or you're not RMP-eligible, you can't use SNAP EBT there for hot food.
However, consider these alternatives:
The answer to "does Popeyes take EBT" is complex.
Navigating EBT rules for fast food can be tricky. The RMP, despite its limits, aims to help vulnerable individuals. For general SNAP info, visit the USDA website:
Whether Popeyes accepts EBT depends on your location and if your state participates in the SNAP Restaurant Meals Program (RMP). This program allows eligible SNAP recipients (elderly, disabled, or homeless individuals in participating states) to use their EBT cards at approved restaurants.
Currently, states known to have Popeyes locations that may participate in the RMP include Arizona, California, Illinois, Maryland, Michigan, Rhode Island, and Virginia. However, participation can vary even within these states, so it's crucial to check with your local Popeyes.
The best way to confirm if a Popeyes location accepts EBT is to call the restaurant directly and ask. You can usually find the phone number through online search engines or the Popeyes website. Look for signage in the restaurant window or at the counter as well.
Eligibility for using EBT at restaurants is typically limited to SNAP recipients who are elderly (60+), have a disability, or are experiencing homelessness, as mandated by the RMP in participating states. Standard SNAP benefits for groceries usually don't cover hot, prepared meals at restaurants for the general population.
Generally, if a Popeyes location participates in the RMP and you are eligible, you can purchase any prepared food item on their menu. There are usually no restrictions on specific menu items for eligible RMP users.
To determine if you qualify for the RMP, contact your local state or county Department of Social Services or the agency that administers SNAP benefits in your area. They can provide information on eligibility criteria and participating restaurants.
If Popeyes doesn't accept EBT, you can use your SNAP benefits at grocery stores and participating farmers' markets to purchase food to prepare at home. Some other fast-food restaurants like Taco Bell, KFC, and Subway may participate in the RMP in certain states; it's best to check with them directly.
Currently, major food delivery platforms like DoorDash or Uber Eats generally do not allow the use of EBT for restaurant meal purchases, even if the restaurant participates in the RMP. EBT is typically restricted to in-person transactions at authorized locations.
Yes, it's always a good idea to inform the cashier that you will be paying with an EBT card before placing your order. This ensures a smooth transaction process and allows them to use the correct payment terminal.
Your state's Department of Social Services or SNAP agency often provides a list or a search tool on their website to find participating restaurants in the RMP. You can also look for signage at restaurants indicating their participation in the program. The USDA's SNAP Retailer Locator might also provide some information, though it primarily focuses on grocery retailers.
Does medicare cover cataract surgery is a common question for many facing vision challenges due to cataracts. The good news is that Medicare generally does provide coverage for this sight-restoring procedure when it's deemed medically necessary by a doctor. This coverage helps pay for the removal of the cataract and implantation of an intraocular lens, significantly improving vision for millions of Americans each year. While Original Medicare (Parts A and B) forms the basis of this coverage, the specifics can vary, and understanding these details is key to managing expectations and potential out-of-pocket costs.
Original Medicare, primarily through Part B (Medical Insurance), covers a range of services related to medically necessary cataract surgery. This ensures that beneficiaries have access to essential treatments to restore vision impaired by cataracts.
The overarching principle guiding Medicare's coverage for cataract surgery is its commitment to restoring functional vision when impaired by a medical condition—the cataract. It is not intended to cover enhancements aimed at achieving perfect vision without glasses or to provide routine eye care, which generally fall outside Medicare's scope. The provision of one pair of corrective lenses post-surgery is a specific, limited benefit directly linked to recovery from the medically necessary procedure.
The cornerstone of Medicare coverage for cataract surgery is "medical necessity." This means the procedure is not considered elective or cosmetic. Instead, an ophthalmologist who accepts Medicare must determine and document that the surgery is essential for the patient's visual health and ability to function.
Criteria for Medical Necessity
Several criteria are used to establish medical necessity, largely focusing on how the cataract impairs a patient's vision and daily life. These guidelines are often detailed in Local Coverage Determinations (LCDs) by Medicare Administrative Contractors, such as LCD L37027.
Visual Acuity and Functional Impairment
While visual acuity measurements, like those from a Snellen eye chart, are part of the examination, they are not the sole determinant for surgery. Medicare guidelines acknowledge that a simple visual acuity score may not fully capture the extent of a patient's functional impairment in real-world conditions, such as when dealing with glare or poor contrast. For instance, a patient might have a Snellen acuity that seems acceptable, yet experiences debilitating glare that makes driving at night impossible.
Therefore, the ophthalmologist's comprehensive assessment of how the cataract affects the patient's overall visual function and quality of life is paramount. Some older guidelines or common understanding might point to a visual acuity of 20/40 (a common threshold for driving in many states) or 20/50 as a benchmark. While such values are often indicative of significant functional impairment, the emphasis is on the broader impact documented by the physician.
Importance of Documentation
Thorough documentation by the ophthalmologist is critical. The medical record must clearly detail the patient's specific complaints, the best-corrected visual acuity, findings from the eye examination, and a description of how the cataract limits the patient's daily activities and overall visual function. This detailed record substantiates the medical necessity of the surgery for Medicare.
Even when Medicare covers cataract surgery, beneficiaries typically have some out-of-pocket expenses. Understanding these costs is essential for financial planning. For those with Original Medicare (Part A and Part B), the primary costs are the Part B deductible and coinsurance.
Factors Influencing Out-of-Pocket Costs
Several factors can influence the total amount a beneficiary will pay out-of-pocket for cataract surgery:
The 20% coinsurance might seem like a manageable percentage, but for cataract surgery, it applies to multiple components (surgeon, facility, lens component). These can accumulate, particularly if a patient requires surgery in both eyes. This cumulative effect highlights why many beneficiaries with Original Medicare choose to enroll in Medicare Supplement Insurance (Medigap) policies, which can cover these coinsurance amounts.
To provide a clearer picture, the following table shows estimated patient costs for cataract surgery with a standard IOL under Original Medicare. It's important to remember these are national averages and actual costs can vary.
Estimated Patient Costs for Cataract Surgery with Original Medicare (Standard IOL)
| Service Setting | Average Total Cost (Medicare-Approved) | Medicare Pays (80%) | Patient Responsibility (20% Coinsurance after Deductible)* | Source Examples |
|---|---|---|---|---|
| Ambulatory Surgical Center (ASC) | ~$1,900 - $2,000 | ~$1,520 - $1,600 | ~$380 - $400 (plus any remaining Part B deductible) | (using 2025 projection) |
| Hospital Outpatient Department | ~$2,900 - $3,000 | ~$2,320 - $2,400 | ~$580 - $600 (plus any remaining Part B deductible) | (using 2025 projection) |
*Note: These are national average estimates for 2024/2025 and can vary based on location, specific services, and provider charges. The Part B deductible ($257 for 2025) must be met before the 20% coinsurance applies.
A critical decision in cataract surgery involves the type of intraocular lens (IOL) that will replace the eye's natural clouded lens. Medicare's coverage differs significantly between standard and advanced (or premium) IOLs.
The type of Medicare plan a beneficiary has significantly influences their coverage details and out-of-pocket costs for cataract surgery.
Choosing between Original Medicare with Medigap versus a Medicare Advantage plan involves weighing factors like premiums, out-of-pocket maximums, network restrictions, and prior authorizations.
Proactive planning and clear communication are essential for a smooth cataract surgery experience with Medicare.
Active patient involvement is crucial, especially when considering premium options or if enrolled in a Medicare Advantage plan.
Post-operative care and understanding benefits for eyewear are important after cataract surgery.
Understanding Medicare coverage for cataract surgery empowers informed decisions.
Understanding these principles helps navigate cataract surgery with Medicare confidently.
Yes, Medicare Part B (Medical Insurance) generally covers cataract surgery when it's deemed medically necessary by a doctor. This includes services like pre-operative exams, the surgery itself, and post-operative care.
Part B usually covers the removal of the clouded lens and the insertion of a standard intraocular lens (IOL). It also includes follow-up care for a certain period after the surgery.
Medicare Part B typically covers the cost of a standard monofocal IOL, which corrects vision at one distance (near, intermediate, or far). If you choose a premium IOL (like toric or multifocal lenses), Medicare will still cover the amount they would have paid for a standard lens, and you'll be responsible for the difference in cost.
While Medicare covers traditional cataract surgery, it may not fully cover the additional costs associated with laser-assisted surgery. You might have to pay an extra out-of-pocket fee for the laser portion.
Medicare Part B doesn't typically cover the cost of eyeglasses or contact lenses needed after cataract surgery. However, if you have a Medicare Advantage plan, it might offer some vision benefits.
Generally, you don't need a referral to see a specialist like an ophthalmologist under Medicare Part B. You can make an appointment directly.
Yes, Medicare Part B covers cataract surgery performed in both hospital outpatient departments and Medicare-certified ambulatory surgical centers. Your out-of-pocket costs might differ depending on the setting.
Yes, under Medicare Part B, you'll typically need to meet your annual deductible before Medicare starts paying its share. After the deductible is met, you'll usually pay 20% of the Medicare-approved amount for the services.
Medicare Advantage plans (Part C) must cover at least as much as Original Medicare (Parts A and B). Many offer additional benefits, but their specific rules, copays, and provider networks can vary, so it's best to check with your plan.
Medicare typically covers medically necessary cataract surgery for each eye, usually performed separately. Each surgery will be subject to the Part B deductible and coinsurance.
Medicare benefits provide foundational health insurance coverage for millions of Americans. Medicare is the federal health insurance program primarily designed for individuals aged 65 and older. However, eligibility extends beyond age; younger people with certain disabilities, permanent kidney failure requiring dialysis or transplant (End-Stage Renal Disease, or ESRD), or Amyotrophic Lateral Sclerosis (ALS, also known as Lou Gehrig's disease) may also qualify for these essential benefits.
The program significantly helps with healthcare costs, but it's important to recognize that it doesn't cover every medical expense, nor does it typically cover the cost of long-term custodial care. Beneficiaries have important choices regarding how they receive their Medicare coverage, influencing costs and access to care. This overview explores who qualifies for Medicare, the different components or "parts" of the program, the primary ways to access coverage, common services included, and the crucial steps for enrollment.
Understanding Medicare eligibility is the first step to accessing benefits. Qualification primarily falls into three categories: age, disability, and specific medical conditions. The Social Security Administration (SSA) is the agency responsible for handling most Medicare enrollment applications and eligibility determinations.
1. Eligibility Based on Age
2. Eligibility Based on Disability
3. Eligibility Based on End-Stage Renal Disease (ESRD)
Medicare is not a single, monolithic plan but is divided into distinct parts, each covering different types of healthcare services. Understanding these parts is crucial for navigating coverage options. Parts A and B are often referred to together as "Original Medicare" and form the foundation of the program.
Part A: Hospital Insurance Benefits
Medicare Part A focuses primarily on inpatient care settings. It helps cover costs associated with:
Part A Costs
Most beneficiaries receive Part A premium-free due to their (or their spouse's) work history. However, "covered" does not mean entirely free. Part A involves cost-sharing, most notably a deductible for each "benefit period" ($1,632 in 2024).
A benefit period begins the day you are admitted as an inpatient and ends once you haven't received inpatient hospital or SNF care for 60 consecutive days. Coinsurance payments are also required for very long hospital or SNF stays within a single benefit period. Those ineligible for premium-free Part A can purchase it if they meet eligibility rules and also enroll in Part B.
Part B: Medical Insurance Benefits
Medicare Part B covers a wide range of medically necessary outpatient services and supplies. Key covered benefits include:
Part B Costs
Unlike Part A, most people pay a monthly premium for Part B. The standard Part B premium amount can change annually, and individuals with higher incomes may pay an Income-Related Monthly Adjustment Amount (IRMAA).
In addition to the premium, Part B generally involves an annual deductible ($240 in 2024). After the deductible is met, beneficiaries typically pay 20% coinsurance for most Part B-covered services and supplies.
Part D: Prescription Drug Coverage
Medicare Part D offers optional coverage specifically designed to help manage the costs of prescription medications. This includes most retail prescription drugs and many recommended vaccines not covered under Part B.
Key aspects include:
Once eligible for Medicare Parts A and B, beneficiaries face a fundamental choice in how they receive their coverage and benefits. The two primary options are Original Medicare or a Medicare Advantage plan.
Original Medicare (Part A & Part B)
This is the traditional fee-for-service program administered directly by the federal government.
Medicare Advantage (Part C)
Medicare Advantage plans offer an alternative way to receive your Part A and Part B benefits, administered through private insurance companies approved by Medicare.
Other Medicare Health Plan Options
While less common, other types of Medicare health plans exist, such as Medicare Cost Plans and Programs of All-inclusive Care for the Elderly (PACE). These plans have unique rules regarding coverage, costs, and provider access. They are typically available only in specific geographic areas.
Comparing Your Main Coverage Choices
The decision between Original Medicare (often paired with Part D and Medigap) and Medicare Advantage involves trade-offs. Original Medicare offers maximum provider flexibility nationwide. Medicare Advantage offers the potential for lower overall premiums, bundled benefits (including drugs), extra perks, and an out-of-pocket maximum, but usually requires using a network. The best choice depends entirely on individual healthcare needs, budget, preferred doctors and hospitals, and lifestyle (e.g., travel frequency).
| Feature | Original Medicare (Parts A & B) | Medicare Advantage (Part C) |
|---|---|---|
| Provider Choice | Can use almost any doctor or hospital that accepts Medicare in the U.S. | Usually must use providers in the plan's network (HMO, PPO) for lowest costs |
| Prescription Drugs | Requires enrolling in a separate Part D plan | Usually included (MA-PD plans) |
| Out-of-Pocket Costs | Pay deductibles & 20% coinsurance; No annual limit for Part A/B costs | Pay plan-specific deductibles, copays, coinsurance; Annual limit on Part A/B costs |
| Supplemental Coverage | Can buy a Medigap policy to cover cost-sharing | Cannot be used with Medigap |
| Extra Benefits | Generally does not cover dental, vision, hearing | May offer routine dental, vision, hearing, fitness benefits |
| Management | Managed by the federal government | Managed by private insurance companies approved by Medicare |
Medicare covers a broad array of hospital and medical services deemed medically necessary. However, coverage isn't automatic for every service. Whether a specific test, item, or service is covered depends on federal and state laws, National Coverage Determinations (NCDs) made by Medicare, and Local Coverage Determinations (LCDs) made by companies processing Medicare claims in specific regions. These decisions often hinge on whether the service is considered reasonable and necessary for diagnosing or treating a medical condition.
Commonly Covered Services
Commonly covered services under Original Medicare (Parts A & B) include:
It's crucial to remember that even when a service is "covered," it usually involves cost-sharing through deductibles, coinsurance, or copayments. This applies unless you have supplemental coverage like Medigap or qualify for assistance programs.
Services Generally Not Covered
Conversely, some services are typically not covered by Original Medicare Parts A and B:
While Original Medicare doesn't cover these, some Medicare Advantage plans may offer partial coverage for dental, vision, or hearing services as an extra benefit.
Enrolling in Medicare at the right time is essential to avoid potential lifelong late enrollment penalties for Part B and gaps in health coverage. Understanding the different enrollment periods is key.
Key Enrollment Periods
How Enrollment Works
Enrollment isn't always automatic.
Enrolling in Part C and Part D
It's important to distinguish enrollment in Parts A and B (handled by SSA) from enrollment in Part C (Medicare Advantage) or Part D (Prescription Drug Plans). Choosing and enrolling in MA or Part D plans involves selecting from private insurance company offerings. This is typically done through the Medicare Plan Finder tool on Medicare.gov or directly with the plan during specific times like your IEP, the annual Open Enrollment Period, or an SEP.
Navigating Medicare benefits can seem complex, but reliable resources are available to provide accurate information and personalized assistance. It is essential to rely on official government sources, as plan details, costs, and rules can change.
Key official resources include:
Medicare benefits offer vital health coverage through various parts (A, B, C, and D) and delivery systems (Original Medicare and Medicare Advantage). Grasping the fundamentals of eligibility, what each part covers, the associated costs, the main ways to receive benefits, and the critical enrollment periods empowers individuals to make choices that best suit their health needs and financial situation.
Because plan availability, costs, and coverage details (especially for Medicare Advantage and Part D plans) can change annually and vary by location, it is crucial to review your options carefully each year. Utilizing the official resources like Medicare.gov and 1-800-MEDICARE is the most reliable way to get accurate, up-to-date information and make informed decisions about your Medicare coverage.
Medicare has four main parts: Part A (hospital insurance) covers inpatient hospital stays, skilled nursing facility care, hospice, and some home health care. Part B (medical insurance) covers doctors' services, outpatient care, preventive services, and some medical equipment. Part C (Medicare Advantage) are plans offered by private companies that contract with Medicare to provide Part A and Part B benefits, often including Part D (prescription drug coverage) and extra benefits. Part D helps pay for prescription drugs.
Generally, you are eligible for Medicare if you are a U.S. citizen or have legally resided in the U.S. for at least 5 years and meet one of these criteria: you are 65 or older and you or your spouse has worked for at least 10 years (40 quarters) in Medicare-covered employment; you are under 65 with a qualifying disability; or you have End-Stage Renal Disease (ESRD) or Amyotrophic Lateral Sclerosis (ALS).
Your Initial Enrollment Period (IEP) starts 3 months before the month you turn 65, includes your birthday month, and ends 3 months after. If you don't enroll during your IEP and don't have creditable coverage (like from a current employer), you may face a late enrollment penalty for Part B that lasts for as long as you have Medicare, and a penalty for Part D if you enroll later.
Most people don't pay a monthly premium for Part A if they or their spouse have the required work history. The standard monthly premium for Part B in 2025 is $185, but this can be higher depending on your income. The deductible for Part A inpatient hospital stays in 2025 is $1,676 per benefit period, and the annual deductible for Part B is $257. After meeting the Part B deductible, you typically pay 20% of the Medicare-approved amount for most doctor services and outpatient care.
Medicare Advantage plans (Part C) are offered by private insurance companies and provide Medicare Part A and Part B benefits, often with additional benefits like vision, dental, and hearing coverage, and sometimes prescription drug coverage (Part D). Unlike Original Medicare, most Medicare Advantage plans have networks of doctors and hospitals you need to use, and they may require prior authorization for certain services. They also have an annual out-of-pocket maximum, which Original Medicare doesn't have.
Medicare Part D is optional prescription drug coverage offered by private insurance companies approved by Medicare. Costs can include a monthly premium, an annual deductible, copayments, or coinsurance, which vary by plan. There are different stages of coverage, including an initial coverage period, a coverage gap (often called the "donut hole"), and catastrophic coverage, each with different cost-sharing rules.
Generally, Original Medicare (Parts A and B) does not cover routine dental care (like cleanings, fillings, or dentures), routine vision care (like eye exams, eyeglasses, or contact lenses), or routine hearing care (like hearing exams or hearing aids). However, some Medicare Advantage plans may offer these additional benefits.
It depends on the size of your employer. If your employer has 20 or more employees, your employer's plan is usually primary, and you may not need to enroll in Part B immediately. However, it's generally recommended to enroll in Part A as it's usually free. If your employer has fewer than 20 employees, Medicare may be primary, and you should likely enroll in both Part A and Part B when you become eligible to avoid coverage gaps.
Yes, several programs can help. Medicaid provides assistance to individuals with low income and resources. Medicare Savings Programs (MSPs) help pay Medicare premiums, deductibles, and coinsurance for those who meet specific income and resource limits. Extra Help is available to assist with Medicare Part D prescription drug costs.
Medigap policies are private insurance plans that help supplement Original Medicare by paying some of the out-of-pocket costs like deductibles and coinsurance. If you have retiree health coverage from a former employer or union, it may coordinate with Medicare to help cover your healthcare costs. It's important to understand whether your retiree coverage pays first or second to Medicare and how it interacts with Medigap if you have both.
Does Wingstop take EBT? Many people wonder if they can use their Supplemental Nutrition Assistance Program (SNAP) benefits at this popular restaurant chain. Generally, Wingstop does not accept Electronic Benefit Transfer (EBT) cards for standard purchases . SNAP benefits are typically meant for buying groceries to prepare at home, not hot, ready-to-eat meals from restaurants.
However, there's a key exception: the Restaurant Meals Program (RMP). This state-run program allows certain eligible SNAP recipients to use their EBT cards at approved restaurants, which can include specific Wingstop locations. Whether you can use EBT at a particular Wingstop depends on several factors.
Understanding EBT and SNAP helps clarify why restaurant purchases are usually restricted.
SNAP aims to supplement food budgets for purchasing staples like fruits, vegetables, meat, dairy, and bread. Hot, prepared foods sold for immediate consumption are typically not eligible under standard SNAP rules.
The Restaurant Meals Program (RMP) is a special part of SNAP designed for specific groups. It's a state option, meaning each state decides whether to offer it. The RMP allows eligible individuals—those who might struggle to prepare meals due to age, disability, or homelessness—to buy prepared meals at approved restaurants using their EBT card.
How Restaurants Join RMP
For a restaurant like Wingstop to participate in the RMP, it must:
Because participation requires these approvals, not all restaurants in an RMP state accept EBT.
Most Wingstop locations cannot accept regular SNAP EBT payments due to federal SNAP rules. The program focuses on grocery items for home cooking. Regulations generally prohibit using SNAP for hot foods sold at the point of sale or intended for immediate consumption, which includes most restaurant food.
Wingstop primarily sells hot, prepared items like wings and fries meant to be eaten soon after purchase. This business model doesn't align with standard SNAP food eligibility rules. Therefore, unless a specific Wingstop is part of the RMP, it cannot process standard EBT payments.
The Restaurant Meals Program creates the pathway for some Wingstop locations to accept EBT. A Wingstop might be authorized if:
This approval is location-specific. For instance, certain Wingstops in California counties like Riverside, Los Angeles, Sacramento, and San Francisco have been approved RMP vendors . However, this doesn't mean all Wingstops in California or other RMP states participate. Each location needs individual authorization.
Furthermore, even at an approved Wingstop, the EBT transaction will only work if the SNAP recipient is eligible for the RMP in their state.
The RMP is optional for states. As of recent information, the following states operate an RMP (though program status can change, so always check official state resources):
Note: This list is based on available data and may change. Verify with your state's official SNAP agency for the most current information.
Not everyone with SNAP in an RMP state qualifies for the program. Eligibility targets those facing challenges in preparing meals. Generally, all members of a SNAP household must fit into one or more of these categories (rules can vary slightly by state ):
State SNAP agencies determine RMP eligibility, not the restaurants.
Since participation varies, you must verify if a specific Wingstop accepts EBT through the RMP. Here’s how:
Remember, seeing Wingstop listed in one area (like Cathedral City, Desert Hot Springs, Los Angeles, Sacramento, or San Francisco ) doesn't guarantee participation elsewhere. Always confirm locally.
At an authorized RMP restaurant, eligible individuals can use their EBT card to buy prepared meals. This typically covers items from the regular menu intended for immediate consumption, like wings, sandwiches, sides, and non-alcoholic drinks sold with the meal.
Standard SNAP restrictions still apply. You cannot use EBT benefits, even under RMP, for:
For customers not using RMP EBT, Wingstop accepts common payment methods, including:
EBT/SNAP is not listed among their standard payment options on official channels , highlighting that acceptance is limited to the RMP exception.
Wingstop isn't the only chain that might participate in the RMP. Depending on state and location approval, others could include:
The same rules apply: participation depends on the state having an RMP, the specific restaurant being authorized, and the customer being RMP-eligible. Always verify first.
For official details on the federal program, visit the USDA's SNAP Restaurant Meals Program.
EBT acceptance at Wingstop is not universal and depends on the specific location and whether the state participates in the Restaurant Meals Program (RMP). In states with RMP, some Wingstop locations may allow eligible individuals to use their EBT cards. It's crucial to check with your local Wingstop directly to confirm if they accept EBT.
The Restaurant Meals Program is a state option within SNAP that allows certain eligible individuals, such as the elderly, disabled, and homeless, to use their EBT cards to purchase prepared meals at participating restaurants. Not all states have this program, and not all restaurants in participating states choose to participate.
The best way to determine if a specific Wingstop location accepts EBT is to call the restaurant directly and ask. You can find the phone number for your local Wingstop on their website or through online search engines. Look for a sign in the restaurant window or near the counter that indicates EBT acceptance.
Generally, SNAP benefits through EBT are intended for staple food items. Prepared, hot foods meant for immediate consumption, like cooked wings and seasoned fries, are typically not eligible for purchase with EBT. However, if a Wingstop location participates in RMP, the rules might differ for eligible individuals. In standard SNAP transactions, you might be able to purchase uncooked chicken or sealed, cold side items if available for takeout. Always confirm with the store about eligible items.
Yes, if a Wingstop accepts EBT through the RMP, it will likely be restricted to eligible individuals (elderly, disabled, homeless) and may have limits on the types of meals that can be purchased. For standard SNAP, the purchase must be for eligible food items, excluding hot, prepared foods.
Wingstop typically accepts cash, credit cards (Visa, MasterCard, American Express, Discover), and debit cards. Some locations may also accept digital payment options like Apple Pay and Google Pay; it's best to confirm with your local store.
Restaurants that participate in the RMP will usually display a sign indicating EBT acceptance. You can also check your state's Department of Social Services website for a list of participating restaurants or use online tools provided by SNAP benefit management apps. Common fast-food chains like McDonald's, Subway, Burger King, and KFC participate in RMP in some locations.
Currently, EBT is generally used for in-store purchases at participating locations. The ability to use EBT for online orders or delivery services like DoorDash varies and is not widely available for most restaurants, including Wingstop. However, some delivery platforms are beginning to pilot EBT acceptance at select grocery stores.
If your EBT card is declined, first ensure that the Wingstop location accepts EBT. If they do, check your EBT account balance to ensure sufficient funds. The card might also be declined if you are attempting to purchase non-eligible items. If you believe the decline is an error, contact your state's EBT customer service number.
No, participation in the Restaurant Meals Program is voluntary for restaurants. Even if a state has the RMP, individual Wingstop franchises can choose whether or not to accept EBT. This is why it's essential to verify with your specific local Wingstop.
Disadvantages of meals on wheels programs, while often outweighed by their significant benefits, are important considerations for potential recipients and their families. Meals on Wheels plays a vital role in supporting the health and independence of many seniors. It provides not just food but also social contact and safety checks.
However, understanding the potential drawbacks is crucial for making fully informed decisions. It helps determine if this service is the right fit for specific needs and circumstances. It is also important to recognize that limitations can vary considerably among the more than 5,000 independent local programs operating across the country. Therefore, investigating local options is essential. This article provides a clear look at these potential limitations.
A significant area of concern for some individuals considering Meals on Wheels revolves around the limitations in meal customization and dietary options. While programs aim to provide nutritious meals, meeting diverse individual needs presents challenges.
Limited Flexibility for Specific Diets
Many Meals on Wheels programs offer options for common dietary needs like diabetic-friendly or low-sodium meals. However, accommodating highly specialized medical diets can be difficult for programs operating on a large scale. This includes complex renal diets beyond basic guidelines, severe food allergies, strong personal preferences (like veganism or specific textures not officially offered), or strict cultural and religious requirements.
Programs funded under the Older Americans Act (OAA) must provide meals meeting specific nutritional standards. These meals must supply at least one-third of the daily Dietary Reference Intakes (DRIs) and comply with the current Dietary Guidelines for Americans (DGAs). While these guidelines set a nutritional baseline and encourage tailoring to preferences and culture , practical customization is often limited. Standardization is necessary for efficiency and cost control.
Some programs explicitly warn about potential cross-contamination, particularly concerning severe allergies like nuts, as kitchens may not be entirely free of allergens. Furthermore, requesting the exclusion of certain ingredients might lead to repetitive side dishes. It could also result in receiving a generic substitute, like a chicken or beef patty, instead of the planned main course.
Menu Variety and Food Quality Concerns
Lack of variety in the menu can lead to dissatisfaction or "menu fatigue" over time for some recipients. Concerns about food quality, specifically taste and texture, are sometimes raised. Descriptions like "bland" may stem from necessary dietary modifications, such as reduced sodium content required for health reasons.
Changes in texture can also occur when food is prepared in bulk, transported, and reheated. While programs strive to provide appealing meals , audits in some locations have occasionally noted recipient complaints regarding meal quality. This indicates that maintaining consistent quality across large operations can be challenging.
Potential Nutritional Gaps
The standard requirement for OAA-funded meals is to provide at least one-third of the daily DRIs. This means recipients must obtain the remaining two-thirds of their necessary nutrients from other sources. This structure positions Meals on Wheels as a supplemental service, not a complete nutritional solution.
For individuals who have difficulty shopping or preparing other meals, this can create significant nutritional gaps. This is especially true on weekends or days without delivery. Studies show participant diet quality can be lower on days they don't receive a program meal, highlighting reliance and potential inadequacy.
Additionally, while meals are often controlled for sodium , concerns may arise about preservatives in some pre-prepared meals. The lack of specific micronutrients like fiber or certain vitamins can also be an issue.
Consistency and accessibility of meal delivery are crucial aspects of the Meals on Wheels service, but several factors can create challenges.
Delivery Inconsistency
While programs work hard to ensure dependable service , deliveries can sometimes be disrupted. Factors such as severe weather, traffic delays, logistical problems, or volunteer availability fluctuations can cause delays or changes in delivery times. For individuals dependent on receiving their meal at a specific time, this unpredictability can be problematic.
The COVID-19 pandemic also forced significant shifts in delivery models. Many programs reduced daily hot meal deliveries, moving towards less frequent drop-offs of frozen or shelf-stable meals for safety and capacity management. Some programs anticipate these pandemic-related changes may become permanent.
Missed Deliveries and Accuracy Issues
There have been reports of recipients not receiving scheduled meals, despite program records indicating completed delivery. Issues can also arise from delivery personnel not following specific instructions, like failing to call if the recipient doesn't answer. Delivering meals to the wrong address, especially in large apartment complexes, has also occurred.
Oversight audits have sometimes found discrepancies, such as programs being paid for unconfirmed deliveries and delays in resolving complaints about missed meals. Such inconsistencies undermine nutritional support and the vital safety check aspect of the service.
Geographic Accessibility Barriers
Providing service to individuals in remote or rural areas presents significant logistical and financial hurdles. The cost and time involved in reaching sparsely populated locations can limit program reach. Similarly, accessing clients in certain urban areas perceived as high-crime can also pose challenges for delivery operations.
Significant Waitlists
Perhaps one of the most critical disadvantages currently is the prevalence of extensive waitlists. This is driven primarily by insufficient funding that hasn't kept pace with rising demand (especially post-COVID-19). Increased food and operational costs due to inflation and persistent volunteer shortages also contribute.
Nationally, reports indicate about one in three Meals on Wheels programs had a waitlist in 2023, an increase from previous years. The average wait time is often around three months, but can extend to years in some areas. This delay is concerning as individuals seeking Meals on Wheels are often already vulnerable. They experience poorer health, higher rates of depression and anxiety, and increased fall risk compared to the general older adult population.
Their health can deteriorate further while waiting for essential nutritional support. This potentially leads to costly hospitalizations or premature placement in nursing homes. These waitlists represent a fundamental gap between the recognized need and available resources.
A frequently highlighted benefit of Meals on Wheels is the social contact provided during meal delivery. However, the nature and extent of this interaction have limitations.
The Value and Brevity of Visits
The interaction between the delivery person (often a volunteer) and the recipient serves as a valuable touchpoint and safety check. For many homebound seniors, this brief visit might be their only social contact all day, making it incredibly important for their sense of connection. Research confirms Meals on Wheels recipients are often socially isolated, a condition linked to serious negative health outcomes like depression, cognitive decline, and increased mortality.
However, the primary purpose of the visit is meal delivery, meaning the social interaction is typically brief. While meaningful connections can form over time , this short encounter may not be sufficient to alleviate deep feelings of loneliness for those with very limited social networks. There can be a mismatch between the perceived social benefit and the capacity of a quick delivery stop to address significant social needs.
Impact of Delivery Models
Furthermore, the trend towards less frequent deliveries, such as weekly drop-offs of frozen meals, inherently reduces opportunities for social interactions and safety checks. This operational shift, while sometimes necessary for efficiency or safety, can diminish the "more than a meal" aspect focused on social well-being.
Supplementary Social Programs
Recognizing this limitation, many Meals on Wheels organizations offer supplementary social connection programs. These might include friendly visiting (longer visits), telephone reassurance calls, pet assistance programs, or group activities. Studies indicate these targeted programs can effectively reduce feelings of social disconnectedness.
However, these are typically add-on services, dependent on additional funding and volunteer resources. They may not be available through all local providers or utilized by all clients who could benefit. Therefore, relying solely on the meal delivery itself for social support represents a potential disadvantage.
Navigating the costs and eligibility requirements for Meals on Wheels can sometimes present challenges for potential recipients, while the programs themselves face significant funding constraints.
Potential Costs for Recipients
OAA-funded programs cannot charge eligible seniors a mandatory fee or deny service based on inability to pay. However, they often rely heavily on voluntary contributions or donations from participants. Some programs may implement a sliding scale fee structure based on income or circumstances.
For individuals not meeting OAA eligibility (e.g., under 60, not homebound) or wanting extra meals, private pay options usually exist, requiring full payment. Even small requested donations can be a burden for seniors on limited incomes. This complex funding mix means the actual cost can vary and may not align with the perception of the service being entirely "free".
Eligibility Requirements
The primary federal eligibility criterion for OAA nutrition programs is age 60 or older. Programs often target individuals who are homebound due to illness or disability, meaning they have difficulty leaving home without help or face challenges shopping and cooking. Specific rules and assessment processes vary by state and local provider.
These criteria, particularly the "homebound" definition, can act as gatekeepers. They might exclude individuals with substantial nutritional risks or meal preparation difficulties (e.g., cognitive impairment, severe arthritis) who don't strictly meet the homebound definition. Programs prioritize serving those in "greatest social and economic need," potentially involving assessments.
Systemic Funding Constraints
Meals on Wheels programs operate on a complex funding model. They rely on federal OAA grants, state/local government funding, private donations, foundation grants, and client contributions. Federal funding often covers only a portion of actual costs.
Critically, this funding hasn't kept pace with the growing number of seniors needing services, rising operational costs, and inflation. Chronic underfunding relative to need is a root cause of many disadvantages, leading to service limitations, program instability, and waitlists. Sudden funding freezes or budget cuts can have immediate, severe impacts, forcing programs to reduce services or turn away eligible seniors. Financial sustainability remains a persistent challenge.
Cost-Effectiveness Comparison
Despite potential costs, Meals on Wheels remains highly cost-effective compared to institutional care.
Illustrative Cost Comparison: Meals on Wheels vs. Institutional Care (Annual Estimate)
| Service Type | Estimated Annual Cost* |
|---|---|
| Meals on Wheels (1 meal/day, 5 days/week) | ~$2,800 - $3,000 |
| Nursing Home Stay (Semi-private room) | ~$94,000+ |
| Hospital Stay (Average cost per day) | ~$2,800+ |
*Note: These figures are illustrative estimates based on various sources and can vary significantly based on location, specific program costs, and individual care needs. They are intended to provide general context.
This comparison highlights that even with some associated costs, the overall expense is dramatically lower than alternatives like nursing homes or extended hospital stays. This supports its role in helping seniors age in place.
It is vital to understand the specific scope of services provided by Meals on Wheels. While invaluable for nutritional support, it is not designed to be a comprehensive care solution.
Scope of Services
The program's core function is delivering nutritious meals and providing brief social contact and safety checks. Meals on Wheels typically does not include assistance with personal care tasks (Activities of Daily Living - ADLs) like bathing, dressing, or toileting. It also doesn't encompass medication management, medical treatments, wound care, or other skilled nursing services.
Services Generally Not Included
Services like housekeeping, transportation for appointments (though some local programs offer limited transport as an add-on ), or in-depth case management are generally outside standard MOW offerings.
Need for Additional Support
Individuals requiring assistance beyond meal delivery and brief check-ins need to arrange these services separately. This might involve hiring private home care aides, using home health agencies, relying on family caregivers, or accessing other community support programs.
A potential disadvantage arises if families mistakenly assume Meals on Wheels provides broader support than it does. This misunderstanding can lead to dangerous gaps if other necessary services aren't arranged. Meals on Wheels is a crucial component of a senior's care plan but rarely suffices alone for those with complex needs.
The operational model of many Meals on Wheels programs relies heavily on the dedication of volunteers, particularly for meal delivery. While some programs use paid drivers or a mix , the volunteer workforce is often critical for service levels and cost control.
Volunteer Recruitment and Retention Challenges
This reliance introduces inherent fragility. Recruiting and retaining enough volunteers is an ongoing challenge. National trends show declines in formal volunteerism, further straining resources. Volunteer shortages directly impact operations: staff may divert time to deliver meals, increasing costs and burnout; routes may consolidate or delivery frequency reduce; programs may struggle to expand or reduce waitlists.
Volunteer Demographics and External Factors
The volunteer base's demographic makeup is also a factor. Historically, many volunteers are older adults themselves. This became problematic during the COVID-19 pandemic, as many high-risk older volunteers had to stop, causing significant workforce disruption.
This vulnerability highlights how service consistency is tied to fluctuating unpaid labor availability. This is influenced by demographics, economics, public health crises, and other external events. Volunteer shortages create a difficult cycle: fewer volunteers increase strain, potentially impacting service quality, making recruitment harder, and ultimately exacerbating waitlists.
Ensuring food safety is paramount, and Meals on Wheels providers must adhere to stringent requirements from health departments and OAA guidelines. However, preparing meals centrally and delivering them introduces potential safety risks.
Program Standards and Oversight
Programs must maintain rigorous standards in kitchens and during transport to control temperature and prevent contamination. Despite these efforts, audits have occasionally identified recurring food safety concerns at some provider sites. Issues like pest activity or failures to prevent contamination underscore the need for consistent oversight and corrective action.
Recipient Handling and Vulnerability
Beyond program control, safety also depends on proper handling by the recipient. Meals, especially frozen ones needing storage and reheating, must be handled correctly to prevent bacterial growth. Programs typically provide instructions, like refrigerating meals promptly.
Ensuring recipients follow guidelines can be challenging, especially for those with cognitive impairments, physical limitations, or inadequate facilities. Older adults, particularly those with underlying health conditions, are more susceptible to foodborne illnesses, making adherence crucial. This "last mile" of food safety within the recipient's home represents an inherent vulnerability.
Meals on Wheels provides invaluable support to millions of older adults. It delivers essential nutrition, vital social contact, and safety checks, enabling many to live independently. However, approaching this service requires understanding its potential disadvantages.
Limitations in dietary customization and menu variety may challenge those with specific needs. Delivery schedules can be inconsistent, and significant waitlists exist due to funding shortfalls and high demand. While social interaction during delivery is beneficial, its brevity may not fully address severe loneliness.
Costs can be a factor depending on the program and circumstances, and eligibility requirements may exclude some. Meals on Wheels focuses on nutrition and isn't a substitute for comprehensive care. Reliance on volunteers creates operational vulnerabilities, and food safety requires constant vigilance from provider and recipient.
These drawbacks highlight the importance of research based on individual needs and local provider offerings. Services, costs, menus, eligibility, and waitlists vary significantly. Contacting the local provider directly is crucial. Exploring all community resources and integrating meal delivery into a broader care plan ensures comprehensive support.
While Meals on Wheels aims to provide nutritious meals, they may not always meet the specific and complex dietary needs of every individual, potentially lacking in certain nutrients or not tailored for specific health conditions like diabetes or kidney disease. Individualized meal planning and more diverse options could improve this.
The primary focus is food delivery, which can mean limited social interaction for recipients, potentially increasing feelings of loneliness, especially for those who rely on the service as a main point of contact. Implementing social dining programs or training drivers to engage in brief conversations could help.
Accessibility can be a challenge, particularly for individuals in rural areas or those lacking reliable transportation, creating barriers to receiving the service. Expanding delivery routes and exploring alternative transportation solutions are potential remedies.
Programs often face funding constraints, which can impact their ability to meet growing demands and provide comprehensive services in the long term. Increased public and private funding is crucial for sustainability.
The service primarily focuses on food delivery and may not address other essential needs such as transportation to appointments, health monitoring, or access to social services. A more holistic approach could be beneficial.
Due to high demand and limited resources, many Meals on Wheels programs have significant waiting lists, leaving some vulnerable seniors without timely access to meals. Increased funding and volunteer recruitment are needed to reduce these wait times.
Some recipients might find the meals bland or not to their personal taste, which could lead to reduced food intake and nutritional benefits. Offering more menu variety and considering dietary preferences could improve satisfaction.
Fixed delivery schedules might not suit everyone, and delays can occasionally occur, affecting meal quality and convenience. More flexible delivery options or better communication could address this.
While programs follow food safety guidelines, there's a potential risk if meals are not kept at the correct temperature during delivery or if recipients are not home to receive them promptly. Clear guidelines and timely delivery are important.
While providing crucial support, over-reliance on meal delivery without other forms of engagement or support could potentially limit opportunities for recipients to maintain their independence in the long run. Encouraging participation in other activities and providing additional support services can help mitigate this.
Losing your job-based health insurance can be stressful. It adds uncertainty during an already challenging time. If you're in Texas facing job loss or reduced hours affecting your health coverage, you might have options to temporarily continue your plan. Understanding these choices is key to maintaining healthcare access.
This article explains the main ways Texans can potentially keep group health benefits after coverage ends. We'll cover federal COBRA and Texas state continuation laws. This includes who qualifies, coverage duration, costs, enrollment, and comparisons to alternatives like the Health Insurance Marketplace.
What is Federal COBRA? (The Basics)
COBRA stands for the Consolidated Omnibus Budget Reconciliation Act. It's a federal law, not an insurance company. COBRA gives eligible workers and families the right to temporarily continue their job-based group health benefits after certain events cause coverage loss. Think of it as a safety net during transitions, like between jobs.
A key feature is that COBRA coverage is generally the same health plan you had while employed. This often means keeping the same doctors and benefits, providing valuable continuity of care.
Which Texas Employers are Subject to COBRA?
Federal COBRA doesn't apply to all employers. In Texas, it generally covers private-sector employers with 20 or more employees on most business days in the previous year. Both full-time and part-time employees count towards this threshold.
COBRA also applies to state and local government group health plans. However, it excludes plans from the federal government or certain church-related organizations. If your employer had fewer than 20 employees, federal COBRA likely won't apply, but Texas law might offer other options.
Who Can Get Federal COBRA Coverage in Texas? (Qualifying Individuals & Events)
To qualify for federal COBRA in Texas, three conditions usually must be met :
Qualified Beneficiaries
These individuals can elect COBRA:
Eligible dependents can elect COBRA even if the former employee doesn't.
Qualifying Events
These specific triggers cause coverage loss and grant COBRA eligibility:
What Types of Health Plans Does COBRA Cover?
COBRA applies to an employer's group health plan. This usually includes medical insurance. If you had separate dental or vision plans through your employer before the event, COBRA generally allows continuing those too. COBRA continuation is limited to the health, dental, and/or vision benefits you had previously.
COBRA only covers health-related benefits. It doesn't extend to other benefits like life or disability insurance.
Understanding federal COBRA specifics like duration, cost, and enrollment is vital.
How Long Does Federal COBRA Coverage Typically Last?
The duration depends on the qualifying event:
Extensions
The 18-month period can sometimes be extended:
Generally, 36 months is the maximum federal COBRA duration.
Calculating the Cost of COBRA Insurance in Texas
COBRA offers continuity but is often expensive. You typically pay the entire premium, including both your previous share and the employer's contribution.
Plans can also charge an administrative fee up to 2%. This means the total cost can be 102% of the plan's cost. Since employers often subsidize heavily, COBRA premiums can be much higher than payroll deductions. Monthly costs can range from $400-$700+ per person. Tobacco use surcharges may also apply.
How to Elect Federal COBRA Coverage
Enrolling involves specific steps and strict deadlines. Missing one can mean losing your rights.
Once elected and the first payment is made, coverage is retroactive, ensuring no gap.
What if your Texas employer is too small for federal COBRA? Texas laws might offer continuation options.
Health Insurance Options if Your Texas Employer is Small
Texas state law provides continuation rights, sometimes called "Texas Mini-COBRA." This is mainly for employees of smaller businesses not subject to federal COBRA. It typically applies to employers with 2 to 19 employees. Some sources mention up to 50, but 2-19 is common for this specific pathway.
Who Qualifies for Texas State Continuation?
Eligibility differs from federal COBRA:
How Long Does Texas State Continuation Last?
If eligible and not qualifying for federal COBRA, Texas state continuation allows keeping group coverage for up to nine months after original coverage ends.
What Does Texas State Continuation Cost?
Cost is similar to federal COBRA. You pay the full premium. Texas law allows up to 102% of the group rate (full premium + 2% admin fee).
Applying for Texas State Continuation
Enrollment involves these steps:
Texas law offers another continuation benefit for some individuals after their federal COBRA coverage ends.
Extending Health Coverage After COBRA Ends in Texas
Texas law allows certain individuals who have exhausted their maximum federal COBRA coverage (18, 29, or 36 months) to continue group coverage for an additional six months. This is separate from the nine-month "Mini-COBRA."
Crucially, like Mini-COBRA, this extension is only available if the plan under COBRA was a fully insured plan subject to Texas insurance laws. It doesn't apply to self-funded plans.
Eligibility and How to Apply for the Extension
To qualify for the six-month extension:
The application process typically involves:
This extension offers a bridge for those on fully insured plans needing more time post-COBRA, but requires proactive application.
Understanding the differences between Federal COBRA, Texas Mini-COBRA, and the Texas Post-COBRA Extension is key.
| Feature | Federal COBRA | Texas State Continuation (Mini-COBRA) | Texas 6-Month Post-COBRA Extension |
|---|---|---|---|
| Applies To Employers | 20+ Employees | 2-19 Employees (Typically) | Employers offering Fully Insured Plans |
| Plan Type | All Group Health Plans (Insured & Self-Funded) | Fully Insured Plans Only | Fully Insured Plans Only |
| Typical Duration | 18-36 Months (depends on event/extensions) | Up to 9 Months | Up to 6 Months (After COBRA ends) |
| Cost Basis | Up to 102% of Full Premium | Up to 102% of Full Premium | Up to 102% of Full Premium (Implied) |
| Key Eligibility Trigger | Qualifying Event (Job Loss, Reduced Hrs, etc.) | Loss of Coverage, Not COBRA Eligible, 3 Mos Prior Coverage | Exhaustion of Federal COBRA |
| Election Window | 60 Days from Notice/Loss of Coverage | 60 Days from Termination/Notice | Apply Before COBRA Ends (often within 30 days) |
Note: Always verify specific details with your plan administrator or the Texas Department of Insurance.
While continuing your existing plan offers familiarity, weigh it against other potential options.
Is COBRA or State Continuation Always the Best Choice?
The main advantage is keeping the same health plan. This means maintaining your doctor network and predictable coverage. However, this comes at a high cost – often the full premium plus an admin fee. Explore potentially cheaper alternatives before enrolling.
Considering the ACA Health Insurance Marketplace (Healthcare.gov)
Losing job-based insurance is a "qualifying life event". This triggers a Special Enrollment Period (SEP), allowing enrollment in a Marketplace plan outside Open Enrollment. In Texas, use Healthcare.gov.
This SEP generally lasts 60 days from losing job-based coverage. Act within this window. Applying via Healthcare.gov also checks eligibility for low-cost/free Medicaid or CHIP.
COBRA/State Continuation vs. Marketplace: A Cost Comparison
This is often the deciding factor.
Due to subsidies, a Marketplace plan could be much cheaper. Visit Healthcare.gov, enter your info, and compare costs against your COBRA/state continuation notice.
Can You Switch from COBRA to the Marketplace?
Switching rules are specific :
Confirm your Marketplace plan's start date before canceling COBRA to avoid coverage gaps.
Keep these factors in mind when navigating health insurance continuation.
How COBRA/State Continuation and Medicare Work Together
Interactions are complex and depend on timing:
Consult your plan administrator and Medicare if eligibility is a factor.
The Importance of Paying Premiums On Time
This is critical. Pay COBRA or state continuation premiums on time. While there's usually a 30-day grace period (after the first payment) , failing to pay fully before it expires will likely cause permanent coverage termination. Cancellation is often retroactive. Once canceled for non-payment, reinstatement is generally impossible. Set reminders.
Verifying Plan Type (Fully Insured vs. Self-Funded)
Eligibility for Texas state continuation (Mini-COBRA and the 6-month extension) depends on plan type.
How to find out your plan type:
Knowing the plan type is essential before assuming eligibility for Texas state continuation.
Navigating these options can be overwhelming. Use these official resources:
Losing employer health insurance in Texas offers several paths. Federal COBRA (for employers with 20+ employees) lets you continue your exact coverage for 18-36 months, but often at high cost (up to 102% premium).
If your smaller employer (2-19 employees) had a fully insured plan, Texas Mini-COBRA might offer nine months of coverage at full cost. If you exhaust federal COBRA from a fully insured plan, Texas law may grant a six-month extension. State options don't apply to self-funded plans.
Crucially, compare these options with the Health Insurance Marketplace (Healthcare.gov). Losing job coverage triggers a 60-day Special Enrollment Period. Marketplace plans might be much cheaper due to potential income-based subsidies.
Consider eligibility, duration, benefits, and cost. Review notices promptly, compare premiums, use official resources, and meet deadlines. Acting quickly and making an informed choice helps maintain vital health coverage.
COBRA (Consolidated Omnibus Budget Reconciliation Act) is a federal law requiring most employers with 20 or more employees to offer continued health coverage to employees and their dependents who would otherwise lose it due to certain qualifying events, such as job loss or reduced hours. In Texas, this means you can temporarily maintain your existing employer-sponsored health plan.
Eligibility extends to employees who were covered under their employer's group health plan and experienced a qualifying event. Dependents (spouses and children) covered under the plan the day before the qualifying event are also eligible, even if the employee doesn't elect COBRA. Qualifying events for employees include termination (for reasons other than gross misconduct) and reduced hours.
For spouses and dependent children, qualifying events include the employee's death, divorce or legal separation from the employee, the employee becoming entitled to Medicare, or a child ceasing to meet the plan's definition of a dependent (e.g., reaching a certain age).
Generally, COBRA coverage lasts for 18 months when the qualifying event is the employee's termination or reduction in hours. However, coverage can extend to 36 months in cases of the employee's death, divorce or legal separation, the employee's Medicare entitlement, or a dependent child losing dependent status.
Yes, a disability extension may allow for an additional 11 months (totaling 29 months) of coverage if the Social Security Administration determines that the qualified beneficiary was disabled at any time during the first 60 days of COBRA coverage and remains disabled. A second qualifying event within the initial 18 months can also extend coverage for dependents up to 36 months.
COBRA coverage is usually more expensive than active employee coverage because you pay the entire premium yourself, including the portion your employer previously covered, plus a potential administrative fee (up to 2%). The exact cost depends on your former employer's group health plan rates. For 2025, the average monthly premium for individual health insurance in Texas is around $509, but your COBRA cost will be based on your specific prior plan.
Your former employer or their benefits administrator must send you a COBRA election notice within 45 days of the qualifying event. You then have 60 days from the date of the notice (or the date coverage ends, whichever is later) to elect COBRA coverage. Enrollment involves completing and returning the election form and making the initial premium payment, which is often retroactive to the date your previous coverage ended.
No, under COBRA, the continuation coverage must be identical to the coverage you had under the group health plan immediately before the qualifying event. You cannot choose a different plan or add new benefits that were not part of your previous coverage.
COBRA maintains your existing coverage and provider network, which can be beneficial if you want to keep your doctors. However, it's often more expensive than Marketplace plans, where you might be eligible for subsidies based on your income. The Marketplace offers a variety of plans, allowing you to choose coverage that best fits your current needs and budget. You can enroll in a Marketplace plan within 60 days of losing your job-based coverage, even if you initially elect COBRA.
Yes, Texas has a "state continuation" law that may apply to employers with 2 to 50 employees who are not subject to federal COBRA. This law allows for continued coverage for up to nine months under certain conditions. It's important to note that state continuation applies to group health benefit plans issued by insurance companies and HMOs subject to the Texas Insurance Code and does not cover self-funded (ERISA) plans.
Florida's Temporary Assistance for Needy Families (TANF) program, also known as Temporary Cash Assistance (TCA), provides crucial support to families facing financial challenges. This article outlines the expected payment schedule, eligibility criteria, and application process for Florida TANF payments in January 2025. Understanding these details can help families access the assistance they need.
Florida TANF payments are typically distributed monthly via the Florida Electronic Benefits Transfer (EBT) card, known as Florida ACCESS. The payment schedule in Florida is based on the last two digits of the recipient's case number. Payments are released throughout the month, starting on the 1st for case numbers ending in 00-03 and concluding on the 28th for case numbers ending in 96-99.
Florida TANF Payment Schedule (Based on Case Number)
To be eligible for TANF in Florida, applicants must meet several criteria. These requirements ensure that assistance is directed to those who need it most while promoting self-sufficiency. Key eligibility factors include:
Applying for TANF in Florida involves a straightforward process with multiple options for submission. The quickest method is through the online ACCESS Florida website. Applicants can also apply through other means:
The application process generally includes these steps :
Upon approval, eligible individuals will receive an Electronic Benefits Transfer (EBT) card to access their monthly benefits.
The amount of the Florida TANF payment varies based on family size and income. For children with no countable income, the monthly payments in 2024 were:
Estimated payment ranges for January 2025, as reported by a non-official source, are :
For the most accurate and up-to-date payment amounts, it is crucial to consult the official Florida Department of Children and Families website.
Florida primarily delivers TANF payments monthly through direct deposit onto the Florida Electronic Benefits Transfer (EBT) card, known as Florida ACCESS . This allows recipients to use a debit-like card to access their benefits at authorized retailers and ATMs. While state statutes allow for other payment methods like state warrants or payments to alternative payees , the EBT card system is the standard method for distributing temporary cash assistance.
There have been reports of a $450 direct deposit expected in January 2025 for Florida families receiving TANF . This payment was reportedly intended to help with back-to-school expenses. However, official announcements from the Florida Department of Children and Families (DCF) regarding this specific payment for January 2025 are currently unavailable on their website . News reports from 2022 indicate a one-time $450 payment per child was distributed to certain families, including TANF recipients, using funds from the American Rescue Plan (CARES Act) . This payment was distributed in mid-July 2022 . Therefore, the reported January 2025 direct deposit might be related to this past initiative or could be inaccurate. It is recommended to monitor the official DCF website for any updates or clarifications.
For the most reliable and current information regarding Florida TANF payments, eligibility, and application procedures for January 2025, please refer to the official website of the Florida Department of Children and Families: https://www.myflfamilies.com/
Your TANF payment should arrive based on the last two digits of your case number, with distribution occurring from January 1st through January 28th. Check the provided schedule to find your specific payment date.
While some sources mention a $450 direct deposit, there is no official confirmation from the Florida Department of Children and Families (DCF) for January 2025. This may refer to a previous one-time payment.
The exact amount varies based on your family size and income. You can find estimated ranges, but the most accurate information will be available through your Florida ACCESS account or by contacting the DCF.
To be eligible, you generally need to be a Florida resident, a U.S. citizen or qualified non-citizen, have a child under 18 living with you, and meet specific income and asset limits. There are also work requirements for most adults.
You can apply online through the ACCESS Florida website, in person at a DCF service center, or by submitting a paper application. The online application is generally the quickest method.
You will likely need to provide proof of identity, residency, income, and Social Security numbers for all household members. Additional documents may be required based on your specific situation.
The standard processing time for a TANF application in Florida can take up to 30 days. It may take longer if a disability determination is needed.
TANF payments in Florida are primarily delivered monthly via direct deposit onto a Florida Electronic Benefits Transfer (EBT) card, known as Florida ACCESS. This card can be used at authorized retailers and ATMs.
Yes, there is a lifetime limit of 48 months of cash assistance for adults in Florida's TANF program. Child-only cases may have different rules.
The official website of the Florida Department of Children and Families (DCF) is the best source for the most current and accurate information. You can find it at https://www.myflfamilies.com/.
Target EBT unlocks a world of savings on groceries! This convenient option allows you to use your SNAP benefits card (EBT) to purchase approved food items at any Target store nationwide. You can even leverage EBT for online grocery orders with pickup or delivery in select states, making it easier than ever to stretch your budget further while enjoying the shopping experience at Target.
Target is a one-stop shop for many, and now it can be your go-to destination for budget-friendly groceries too! Target EBT allows you to seamlessly utilize your SNAP benefits, also known as the Supplemental Nutrition Assistance Program, at any Target store across the nation. This handy option unlocks a world of savings, making it easier to stretch your grocery budget further.
What is Target EBT?
Target EBT is the integration of SNAP benefits with Target's payment system. If you're a SNAP recipient, you can use your EBT card to purchase authorized food items at Target, just like you would with a debit card. This eliminates the need for separate shopping trips and allows you to enjoy the convenience and variety offered by Target.
Benefits of Using Target EBT
Who Can Use Target EBT?
While Target facilitates EBT purchases, eligibility for SNAP benefits is determined by your state agency. Generally, SNAP eligibility hinges on factors like household income, citizenship status, and work requirements for certain individuals. Check the official SNAP website (https://www.fns.usda.gov/snap/supplemental-nutrition-assistance-program) or reach out to your local SNAP office for more information.
Getting Started with Target EBT
Once you've been approved for SNAP benefits, you'll receive an EBT card. Using your EBT card at Target is straightforward:
The Supplemental Nutrition Assistance Program (SNAP) is a federal program administered by individual states. There are some general eligibility guidelines, but specific requirements may vary by location. Here's a breakdown of some key factors:
Taking the First Step
If these points seem like you might qualify, here's how to find out for sure:
Additional Considerations
While the above provides a general overview, keep these factors in mind:
Target EBT offers a convenient way to utilize your SNAP benefits for grocery purchases at any Target store nationwide. However, to ensure a smooth checkout experience, it's crucial to understand the requirements associated with using your EBT card at Target.
Types of Eligible Purchases
Target EBT allows you to purchase a wide range of SNAP-approved food items, including:
Non-Eligible Items
It's important to note that not all items at Target can be purchased with your EBT card. Here are some common non-eligible categories:
Separating Your Purchases
To avoid any delays or confusion at checkout, it's recommended to separate your SNAP-eligible groceries from any non-eligible items in your cart. This allows the cashier to easily distinguish which items will be paid for with your EBT card.
Payment Methods for Non-Eligible Items
If you have non-eligible items in your cart alongside your SNAP purchases, you can pay for them using a separate payment method, such as a debit card, credit card, or Target gift card.
Additional Fees and Limitations
Understanding Your EBT Balance
It's important to keep track of your remaining SNAP benefits balance on your EBT card. You can usually check your balance online through your state's SNAP portal or at an ATM. Remember, your EBT card cannot be used for purchases exceeding your available SNAP benefits balance.
Target EBT offers a convenient way to utilize your SNAP benefits for groceries, but it's not the only option. Here's a breakdown to help you decide if Target EBT is the best fit for your needs, compared to other stores:
Target EBT Advantages:
Target EBT Considerations:
Alternatives to Target EBT:
Choosing the Right Fit:
The best store for you depends on your individual needs and priorities. Consider these factors:
Here's a quick comparison table to summarize:
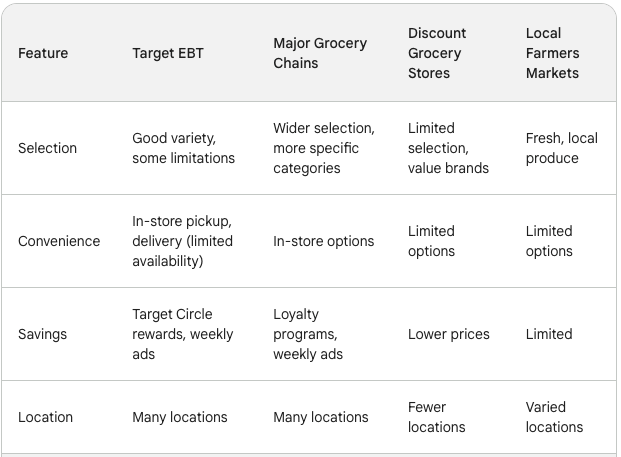
Ultimately, the best way to choose is to explore your options! Visit different stores, compare prices and selection, and see which best suits your needs while maximizing your SNAP benefits.
Here are some top tips to help you become a Target EBT pro:
Master the Art of Combining Savings:
Planning is Key:
Maximize Your Shopping Experience:
Remember:
By following these tips and utilizing Target EBT effectively, you can make the most of your SNAP benefits and enjoy a more budget-friendly grocery shopping experience at Target.
Yes! Target accepts EBT cards at all their physical stores nationwide. You can use your EBT card to purchase a wide range of SNAP-approved food items.
Target EBT for online grocery orders with pickup or delivery is available in select states only. Check the Target website or app for updates on online EBT availability in your area.
Yes! If you have non-SNAP-eligible items in your cart alongside your SNAP purchases, you can pay for them using a separate payment method, such as a debit card, credit card, or Target gift card.
Target itself doesn't charge any fees for using your EBT card. However, delivery or service fees for online grocery orders cannot be paid for with your EBT card. There may also be minimum order requirements for online grocery pickup or delivery, depending on your location and chosen service.
You can usually check your remaining SNAP benefits balance online through your state's SNAP portal or at an ATM. Remember, your EBT card cannot be used for purchases exceeding your available SNAP benefits balance.
Check the Target website or app for the latest information on Target EBT, including online order eligibility updates in your state. You can also sign up for Target emails to receive updates and promotions.
This article provides a good overview of Target EBT requirements. You can also visit the Target website or app for more details.
Many major grocery chains, discount grocery stores, and some local farmers markets accept EBT cards. Consider factors like selection, convenience, and savings when choosing the right store for your needs.